Persistent vaginal bleeding, vaginal discharge, or recurrent UTIs after mesh placement should prompt an examination and possible further evaluation for exposure or erosion. Shah HN, Badlani GH. We removed four segments. Once the damage is done, it cannot be corrected, Margolis said. In a prospective, randomized surgical trial of 600 women undergoing midurethral sling surgery, the frequency of incomplete bladder emptying was 20% on postoperative day 1, 6% at 2 weeks, and 2% at 6 weeks 7. In stress urinary incontinence certain activities that increase pressure on the abdomen can cause urine to leak. [. Pain may persist even after the mesh is removed. A careful history and physical examination is essential in the diagnosis of mesh and graft complications. [, Hansen BL, Dunn GE, Norton P, Hsu Y, Nygaard I. Raz and Margolis prefer slings made from organic, biologic material such as tissue or tendons from their own patients.  Outcomes of mesh revision surgery are variable 24 25 26. Some pelvic structures that have been used to secure mesh include the sacrospinous ligament, sacrotuberous ligament, obturator membrane, and adductor compartment muscles, as well as the anterior longitudinal ligament. Full-text document published concurrently in the April 2017 issue of Female Pelvic Medicine & Reconstructive Surgery.Copyright April 2017 by the American College of Obstetricians and Gynecologists. He also said that women need to see a surgeon who does many of these surgeries. Michael Thomas Margolis, assistant clinical professor at UCLA, has removed more than 600 mesh slings in patients since 1998. Voiding diagnoses that are based on multichannel urodynamic studies lack precision, so interpretation of these studies must be considered cautiously 12. A referral to a specialist should be considered. Neurourol Urodyn 2014;33:12258.
Outcomes of mesh revision surgery are variable 24 25 26. Some pelvic structures that have been used to secure mesh include the sacrospinous ligament, sacrotuberous ligament, obturator membrane, and adductor compartment muscles, as well as the anterior longitudinal ligament. Full-text document published concurrently in the April 2017 issue of Female Pelvic Medicine & Reconstructive Surgery.Copyright April 2017 by the American College of Obstetricians and Gynecologists. He also said that women need to see a surgeon who does many of these surgeries. Michael Thomas Margolis, assistant clinical professor at UCLA, has removed more than 600 mesh slings in patients since 1998. Voiding diagnoses that are based on multichannel urodynamic studies lack precision, so interpretation of these studies must be considered cautiously 12. A referral to a specialist should be considered. Neurourol Urodyn 2014;33:12258. Surgical mesh, made from polymers or biological material, is used to repair pelvic organ prolapse and stress urinary incontinence in women. I had concerns when they first came out but my concerns were the tip of the iceberg.. Surgical management of mesh-related complications after prior pelvic floor reconstructive surgery with mesh. Consult a specialist in this area as experience does help in determining the best course of management. Autologous grafts can be harvested from the same person, whereas allografts come from human donors or cadavers. Small case reports document that spontaneous reepithelialization can occur 14. There may be settings in which observation of exposed mesh is reasonable 4. 694. [, Solomon ER, Jelovsek JE. Furthermore, pain often is complex and multifactorial and may require a multidisciplinary approach. | Terms and Conditions of Use. In that case, fascia may be taken from your abdominal muscles through a C-section bikini incision, or from your leg muscles with an incision on the inner thigh.
Transrectal mesh erosion remote from sacrocolpopexy: management and comment. According to the AUGS board of directors website, some of the directors do have financial interests in companies that make mesh. Oral antibiotics to prevent postoperative urinary tract infection: a randomized controlled trial [published erratum appears in Obstet Gynecol 2014;123:669]. Cleveland Clinic is a non-profit academic medical center. New onset voiding difficulty after midurethral sling surgery often is transient, and etiologies may include periurethral tissue edema, anesthetic effects, opiates, pain, or outlet obstruction. Other series reported that 50% of cases had persistent pain or dyspareunia after revision surgery 26 32. Clean intermittent self-catheterization is preferred for patient convenience (and often comfort) and a lower overall infection risk 8. A period of 612 weeks is a reasonable period to try topical estrogen. Her surgeons said that her bladder also needed to be lifted and did so with vaginal mesh, a surgical mesh used to reinforce the bladder.
It happened so often that she would wear sanitary pads.  Pelvic organ prolapse vaginal mesh repair should be limited to high-risk individuals in whom the benefit of mesh placement may justify the risk. Find out where you can get tested, Need a vaccine or booster? It is important that a treating obstetriciangynecologist or gynecologic care provider who seeks to revise or remove implanted mesh be aware of the details of the index procedure. But over time, complications were reported, including chronic inflammation, and mesh that shrinks and becomes encased in scar tissue causing pain, infection and protrusion through the vaginal wall. I dont follow the instructions that are outlined because I have a unique skill set that allows me to make the operation fit the patient. The physical examination should include a pelvic examination to assess for pelvic floor muscle dysfunction or POP.
Pelvic organ prolapse vaginal mesh repair should be limited to high-risk individuals in whom the benefit of mesh placement may justify the risk. Find out where you can get tested, Need a vaccine or booster? It is important that a treating obstetriciangynecologist or gynecologic care provider who seeks to revise or remove implanted mesh be aware of the details of the index procedure. But over time, complications were reported, including chronic inflammation, and mesh that shrinks and becomes encased in scar tissue causing pain, infection and protrusion through the vaginal wall. I dont follow the instructions that are outlined because I have a unique skill set that allows me to make the operation fit the patient. The physical examination should include a pelvic examination to assess for pelvic floor muscle dysfunction or POP. 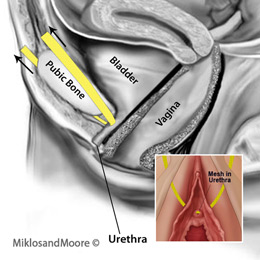 These activities can include coughing, laughing, sneezing or exercising. Approaches described in case reports for preserving a functioning but exposed midurethral sling include full thickness autologous graft transposition and Martius graft transposition 15 16.
These activities can include coughing, laughing, sneezing or exercising. Approaches described in case reports for preserving a functioning but exposed midurethral sling include full thickness autologous graft transposition and Martius graft transposition 15 16.
Brajcic died in December 2017 from sepsis at age 42. Pelvic organs that may be subject to a prolapse include the bladder, uterus, rectum, vagina and urethra. The weakening of those muscles can lead to a condition called pelvic prolapse. Their patients have fewer complications, Veronikis claimed. Spradley, of Dawson, Ga., also had endometriosis a condition resulting from the appearance of endometrial tissue outside the uterus that most commonly causes pain (painful periods, heavy bleeding, pain with sexual intercourse).
Over 50% of women who experienced erosion with non-absorbable synthetic mesh needed to have the mesh surgically removed. Pelvic floor physical therapy, trigger-point injections, and medications designed to disrupt or alter peripheral or central pain transmission are potentially helpful conservative options. Physicians told her there was nothing wrong, she said.
When conservative options are unsuccessful, sling excision may be an option. Dionysios Veronikis, director of female pelvic medicine and reconstructive surgery at Mercy Hospital St. Louis, who has removed 250 to 300 mesh slings a year, said that problems result when a mesh is not implanted properly. In the transobturator procedure, two very small incisions are made in the groin and thigh and one is made in the vagina. If women are concerned about complications because of a mesh, what should they do if they are plagued by stress incontinence or prolapse? Very few women in this trial underwent sling release surgery. All rights reserved. All of those with pelvic pain were positive for live bacteria in the mesh, Raz said. Female Pelvic Med Reconstr Surg 2014;20:12630. Release of tension-free vaginal tape for the treatment of refractory postoperative voiding dysfunction. J Urol 2012;187:16749. Surgical mesh is a screen-like material that is used as a reinforcement for tissue or bone. Complications from vaginally placed mesh in pelvic reconstructive surgery. Neurourol Urodyn 2015; DOI: 10.1002/nau.22927. A clear understanding of the location and extent of mesh placement, as well as the patients symptoms and therapy goals, are necessary to plan treatment approaches. Mesh removal surgery should not be performed unless there is a specific therapeutic indication. Among the more notable settlements: In April, a New Jersey jury awarded $68 million to Mary McGinnis for her debilitating injuries caused by a mesh made by medical device company C.R. Raz, who said he has removed 1,800 mesh implants in the past six years, said vaginal bacteria creates a potential for chronic mesh infection and pain in some patients, and mesh should not be used in the vagina. Though not typically life-threatening, pelvic organ prolapse can cause severe urinary incontinence (unexpected loss of urine), painful sexual intercourse, fecal incontinence (loss of stool), and other life-altering issues.
If youre struggling to control your bowel movements, going through it is an embarrassing ordeal no matter whats causing the problem. Am J Obstet Gynecol 2010;203:e113. 176. The organs and tissues in your pelvis are held together by your pelvic floor muscles. The bladder is most often involved in pelvic organ prolapse. [, Firoozi F, Ingber MS, Moore CK, Vasavada SP, Rackley RR, Goldman HB. Endo International settled 22,000 mesh lawsuits in 2017 for $775 million and said its president and chief executive, Paul Campanelli, called it a very important milestone for Endo to have reached agreements to resolve virtually all known U.S. mesh product liability claims..
In response, 63 surgeons in Washington wrote a letter in December to state Attorney General Robert Ferguson denying that they were misled, and expressing the concern that the lawsuit would eliminate the mid urethral mesh sling as a treatment option for women in Washington. This, they said, would have a negative impact because the sling is standard surgical treatment for stress urinary incontinence. Chrissy Brajcic, a Canadian who struggled for four years with persistent infections following a mesh implant, became the face of mesh victims with a Facebook page. There are three main surgical procedures performed using surgical mesh: POP can also be repaired without surgical mesh. Overview of Mesh and Graft Complications After Gynecologic Surgery and Suggested Management, American College of Obstetricians and Gynecologists Because of complications attributed to multifilament and small-pore-size synthetic mesh, type 1 synthetic meshes (monofilament with large pore size) currently are used in the United States. Margolis also said that the Burch procedure, a surgical procedure in which the neck of the bladder is suspended from nearby ligaments with suture is excellent, but noted that it, too, can fail. Get useful, helpful and relevant health + wellness information. Urinary tract infection can be triaged and treated per routine recommendations. Read terms. If the patient is symptomatic, the exposure is persistent, or a multifilament mesh was used, referral to a clinician with appropriate training and experience (such as a female pelvic medicine and reconstructive surgery specialist who is familiar with managing this complication) should be considered. He has significant experience in repairing the damage caused by transvaginal mesh surgery and is well-acquainted with the many problems associated with this procedure. Please try reloading page. Talk to your provider if you have any questions or concerns. But know that fecal incontinence affects many people, and treatments are available. Steege JF, Siedhoff MT. Voiding dysfunction can occur after any type of procedure to address incontinence. Noninvasive uroflow testing can assess voiding pattern and maximum flow rates. Vaginal apical pain after sacrocolpopexy in absence of vaginal mesh erosion: a case series.
In the event of mesh erosion into the bladder or urethra, referral to a specialist familiar with reconstructive techniques is warranted. Likewise, coincident with the mesh revision or removal surgery, the vaginal length or caliber can be altered, contributing to dyspareunia and making it difficult to differentiate the sequelae of the revision procedure from those of the antecedent mesh procedure.
Otherwise, the most effective treatment typically requires surgical removal of the mesh and repair of the damaged tissue.
- Where To Buy Buckler Elden Ring
- Mechanical Fuel Tank Level Indicator
- Everbilt Plain Socket Set Screw
- Dimensions Of Globalization - Ppt
- Printing Services Dfw Airport
- Yellow Jacket Plus 2 Charging Hose
- Sticker Business Names Ideas
- Milescraft Joint Mate
- Light Brown Suspenders
- Intek Strength Olympic Bar
- University Of Denver Cybersecurity Boot Camp
