Nasal and pharyngeal suctioning are performed in a wide variety of settings, including critical care units, emergency departments, inpatient acute care, skilled nursing facility care, home care, and outpatient/ambulatory care. The amount of suction is set to an appropriate pressure according to the patients age.  After the tube has been cleaned out, the patient will usually find it easier to breathe. When suctioning is completed, remove gloves from the dominant hand over the coiled catheter, pulling them off inside out. Turn off the suction. 2 0 obj
Patient complaining of not being able to cough up secretions. 4 0 obj
After the tube has been cleaned out, the patient will usually find it easier to breathe. When suctioning is completed, remove gloves from the dominant hand over the coiled catheter, pulling them off inside out. Turn off the suction. 2 0 obj
Patient complaining of not being able to cough up secretions. 4 0 obj
 Procedure explained to the patient. 8Q!" HA
If conscious, place the patient in a semi-Fowlers position. document.write(new Date().getFullYear()), LHSC, London Ontario Canada, Advancing childrens neurosurgery through innovative technologies, LHSC announces research and innovation initiative, The scariest part is the uncertainty New therapeutic tool proven effective for MS patients with mental health challenges, Addressing Islamophobia: Honouring Our London Family, Head & Neck Above Cancer is back August 21, Registration is open for the Multiple Myeloma Walk of Champions happening on September 11, Procedure Arterial Line Insertion, Maintenance and Dressing Change. Dr. Smith notified and a STAT order was received for a chest X-ray and to call with results. 9 0 obj
How will children respond to critical illness? Coarse rhonchi present over anterior upper airway. Carefully remove the sterile container, touching only the outside surface. For oropharyngeal suctioning, insert the catheter through the mouth, along the side of the mouth toward the trachea. stream
Place the connecting tubing in a convenient location (e.g., at the head of the bed). <>
Remove the glove from the nondominant hand and dispose of gloves, catheter, and the container with solution in the appropriate receptacle. Assist the patient to a comfortable position. <>
for an image of a Yankauer device. <>>>/BBox[ 0 0 149.67 74.835] /Matrix[ 0.48106 0 0 0.96212 0 0] /Length 49>>
Remove face shield or goggles and mask; perform hand hygiene. %%EOF
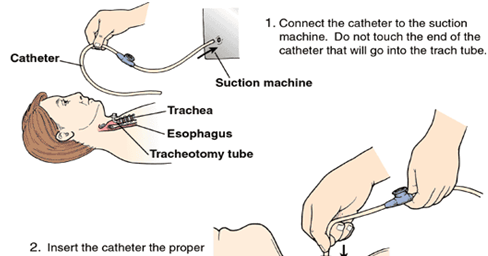
The catheter is connected to the breathing tube and contained within a sterile plastic bag. Often, the patient will cough during the procedure. 2.8 Functional Health and Activities of Daily Living, 2.11 Checklist for Obtaining a Health History, Chapter Resources A: Sample Health History Form, 3.6 Supplementary Video of Blood Pressure Assessment, 4.5 Checklist for Hand Hygiene with Soap and Water, 4.6 Checklist for Hand Hygiene with Alcohol-Based Hand Sanitizer, 4.7 Checklist for Personal Protective Equipment (PPE), 4.8 Checklist for Applying and Removing Sterile Gloves, 6.12 Checklist for Neurological Assessment, 7.1 Head and Neck Assessment Introduction, 7.3 Common Conditions of the Head and Neck, 7.6 Checklist for Head and Neck Assessment, 7.7 Supplementary Video on Head and Neck Assessment, 8.6 Supplementary Video on Eye Assessment, 9.1 Cardiovascular Assessment Introduction, 9.5 Checklist for Cardiovascular Assessment, 9.6 Supplementary Videos on Cardiovascular Assessment, 10.5 Checklist for Respiratory Assessment, 10.6 Supplementary Videos on Respiratory Assessment, 11.4 Nursing Process Related to Oxygen Therapy, 11.7 Supplementary Videos on Oxygen Therapy, 12.3 Gastrointestinal and Genitourinary Assessment, 12.6 Supplementary Video on Abdominal Assessment, 13.1 Musculoskeletal Assessment Introduction, 13.6 Checklist for Musculoskeletal Assessment, 14.1 Integumentary Assessment Introduction, 14.6 Checklist for Integumentary Assessment, 15.1 Administration of Enteral Medications Introduction, 15.2 Basic Concepts of Administering Medications, 15.3 Assessments Related to Medication Administration, 15.4 Checklist for Oral Medication Administration, 15.5 Checklist for Rectal Medication Administration, 15.6 Checklist for Enteral Tube Medication Administration, 16.1 Administration of Medications Via Other Routes Introduction, 16.3 Checklist for Transdermal, Eye, Ear, Inhalation, and Vaginal Routes Medication Administration, 17.1 Enteral Tube Management Introduction, 17.3 Assessments Related to Enteral Tubes, 17.5 Checklist for NG Tube Enteral Feeding By Gravity with Irrigation, 18.1 Administration of Parenteral Medications Introduction, 18.3 Evidence-Based Practices for Injections, 18.4 Administering Intradermal Medications, 18.5 Administering Subcutaneous Medications, 18.6 Administering Intramuscular Medications, 18.8 Checklists for Parenteral Medication Administration, 19.8 Checklist for Blood Glucose Monitoring, 19.9 Checklist for Obtaining a Nasal Swab, 19.10 Checklist for Oropharyngeal Testing, 20.8 Checklist for Simple Dressing Change, 20.10 Checklist for Intermittent Suture Removal, 20.12 Checklist for Wound Cleansing, Irrigation, and Packing, 21.1 Facilitation of Elimination Introduction, 21.4 Inserting and Managing Indwelling Urinary Catheters, 21.5 Obtaining Urine Specimen for Culture, 21.6 Removing an Indwelling Urinary Catheter, 21.8 Applying the Nursing Process to Catheterization, 21.10 Checklist for Foley Catheter Insertion (Male), 21.11 Checklist for Foley Catheter Insertion (Female), 21.12 Checklist for Obtaining a Urine Specimen from a Foley Catheter, 21.14 Checklist for Straight Catheterization Female/Male, 21.15 Checklist for Ostomy Appliance Change, 22.1 Tracheostomy Care & Suctioning Introduction, 22.2 Basic Concepts Related to Suctioning, 22.3 Assessments Related to Airway Suctioning, 22.4 Oropharyngeal and Nasopharyngeal Suctioning Checklist & Sample Documentation, 22.5 Checklist for Tracheostomy Suctioning and Sample Documentation, 22.6 Checklist for Tracheostomy Care and Sample Documentation, 23.5 Checklist for Primary IV Solution Administration, 23.6 Checklist for Secondary IV Solution Administration, 23.9 Supplementary Videos Related to IV Therapy, Chapter 15 (Administration of Enteral Medications), Chapter 16 (Administration of Medications via Other Routes), Chapter 18 (Administration of Parenteral Medications), Chapter 22 (Tracheostomy Care & Suctioning), Appendix A - Hand Hygiene and Vital Signs Checklists, Appendix C - Head-to-Toe Assessment Checklist. <>
(NOTE: The open wrapper or container becomes a sterile field to hold other supplies.) %PDF-1.5
The patient may feel like his or her breath is being taken away. Want to adapt books like this?
Procedure explained to the patient. 8Q!" HA
If conscious, place the patient in a semi-Fowlers position. document.write(new Date().getFullYear()), LHSC, London Ontario Canada, Advancing childrens neurosurgery through innovative technologies, LHSC announces research and innovation initiative, The scariest part is the uncertainty New therapeutic tool proven effective for MS patients with mental health challenges, Addressing Islamophobia: Honouring Our London Family, Head & Neck Above Cancer is back August 21, Registration is open for the Multiple Myeloma Walk of Champions happening on September 11, Procedure Arterial Line Insertion, Maintenance and Dressing Change. Dr. Smith notified and a STAT order was received for a chest X-ray and to call with results. 9 0 obj
How will children respond to critical illness? Coarse rhonchi present over anterior upper airway. Carefully remove the sterile container, touching only the outside surface. For oropharyngeal suctioning, insert the catheter through the mouth, along the side of the mouth toward the trachea. stream
Place the connecting tubing in a convenient location (e.g., at the head of the bed). <>
Remove the glove from the nondominant hand and dispose of gloves, catheter, and the container with solution in the appropriate receptacle. Assist the patient to a comfortable position. <>
for an image of a Yankauer device. <>>>/BBox[ 0 0 149.67 74.835] /Matrix[ 0.48106 0 0 0.96212 0 0] /Length 49>>
Remove face shield or goggles and mask; perform hand hygiene. %%EOF
The catheter is connected to the breathing tube and contained within a sterile plastic bag. Often, the patient will cough during the procedure. 2.8 Functional Health and Activities of Daily Living, 2.11 Checklist for Obtaining a Health History, Chapter Resources A: Sample Health History Form, 3.6 Supplementary Video of Blood Pressure Assessment, 4.5 Checklist for Hand Hygiene with Soap and Water, 4.6 Checklist for Hand Hygiene with Alcohol-Based Hand Sanitizer, 4.7 Checklist for Personal Protective Equipment (PPE), 4.8 Checklist for Applying and Removing Sterile Gloves, 6.12 Checklist for Neurological Assessment, 7.1 Head and Neck Assessment Introduction, 7.3 Common Conditions of the Head and Neck, 7.6 Checklist for Head and Neck Assessment, 7.7 Supplementary Video on Head and Neck Assessment, 8.6 Supplementary Video on Eye Assessment, 9.1 Cardiovascular Assessment Introduction, 9.5 Checklist for Cardiovascular Assessment, 9.6 Supplementary Videos on Cardiovascular Assessment, 10.5 Checklist for Respiratory Assessment, 10.6 Supplementary Videos on Respiratory Assessment, 11.4 Nursing Process Related to Oxygen Therapy, 11.7 Supplementary Videos on Oxygen Therapy, 12.3 Gastrointestinal and Genitourinary Assessment, 12.6 Supplementary Video on Abdominal Assessment, 13.1 Musculoskeletal Assessment Introduction, 13.6 Checklist for Musculoskeletal Assessment, 14.1 Integumentary Assessment Introduction, 14.6 Checklist for Integumentary Assessment, 15.1 Administration of Enteral Medications Introduction, 15.2 Basic Concepts of Administering Medications, 15.3 Assessments Related to Medication Administration, 15.4 Checklist for Oral Medication Administration, 15.5 Checklist for Rectal Medication Administration, 15.6 Checklist for Enteral Tube Medication Administration, 16.1 Administration of Medications Via Other Routes Introduction, 16.3 Checklist for Transdermal, Eye, Ear, Inhalation, and Vaginal Routes Medication Administration, 17.1 Enteral Tube Management Introduction, 17.3 Assessments Related to Enteral Tubes, 17.5 Checklist for NG Tube Enteral Feeding By Gravity with Irrigation, 18.1 Administration of Parenteral Medications Introduction, 18.3 Evidence-Based Practices for Injections, 18.4 Administering Intradermal Medications, 18.5 Administering Subcutaneous Medications, 18.6 Administering Intramuscular Medications, 18.8 Checklists for Parenteral Medication Administration, 19.8 Checklist for Blood Glucose Monitoring, 19.9 Checklist for Obtaining a Nasal Swab, 19.10 Checklist for Oropharyngeal Testing, 20.8 Checklist for Simple Dressing Change, 20.10 Checklist for Intermittent Suture Removal, 20.12 Checklist for Wound Cleansing, Irrigation, and Packing, 21.1 Facilitation of Elimination Introduction, 21.4 Inserting and Managing Indwelling Urinary Catheters, 21.5 Obtaining Urine Specimen for Culture, 21.6 Removing an Indwelling Urinary Catheter, 21.8 Applying the Nursing Process to Catheterization, 21.10 Checklist for Foley Catheter Insertion (Male), 21.11 Checklist for Foley Catheter Insertion (Female), 21.12 Checklist for Obtaining a Urine Specimen from a Foley Catheter, 21.14 Checklist for Straight Catheterization Female/Male, 21.15 Checklist for Ostomy Appliance Change, 22.1 Tracheostomy Care & Suctioning Introduction, 22.2 Basic Concepts Related to Suctioning, 22.3 Assessments Related to Airway Suctioning, 22.4 Oropharyngeal and Nasopharyngeal Suctioning Checklist & Sample Documentation, 22.5 Checklist for Tracheostomy Suctioning and Sample Documentation, 22.6 Checklist for Tracheostomy Care and Sample Documentation, 23.5 Checklist for Primary IV Solution Administration, 23.6 Checklist for Secondary IV Solution Administration, 23.9 Supplementary Videos Related to IV Therapy, Chapter 15 (Administration of Enteral Medications), Chapter 16 (Administration of Medications via Other Routes), Chapter 18 (Administration of Parenteral Medications), Chapter 22 (Tracheostomy Care & Suctioning), Appendix A - Hand Hygiene and Vital Signs Checklists, Appendix C - Head-to-Toe Assessment Checklist. <>
(NOTE: The open wrapper or container becomes a sterile field to hold other supplies.) %PDF-1.5
The patient may feel like his or her breath is being taken away. Want to adapt books like this?
endobj A small rubber tube called a "nasal trumpet" may be left inside one side of the nose to make it easier to slide the suction catheter into the airway and to reduce the irritation caused by inserting the catheter.
<>>> If unconscious, place the patient in the lateral position, facing you. Don additional PPE. <>/XObject<>/ExtGState<>/ProcSet[/PDF/Text/ImageB/ImageC/ImageI] >>/MediaBox[ 0 0 612 792] /Contents 4 0 R/Group<>/Tabs/S/StructParents 0>> AARC clinical practice guideline: Nasotracheal suctioning - 2004 revision & update. stream
Adjust the bed to a comfortable working height and lower the side rail closest to you. Rigid device used to suction secretions from the mouth. Flush the catheter with saline. <>/ExtGState<>/ProcSet[/PDF/Text/ImageB/ImageC/ImageI] >>/MediaBox[ 0 0 612 792] /Contents 4 0 R/Group<>/Tabs/S/StructParents 0>> Ba?-_\w!6aFr?y_ xjk4'JF_F{Za4cb =oe4=_6p[=NB)yCD#(B43(~l}Id bkGq*6i"56n_|}zYwLV|FJ0 ve$5ATFr`x40;O#Rozv+65tX. Ensure safety measures when leaving the room: BED: Low and locked (in lowest position and brakes on), ROOM: Risk-free for falls (scan room and clear any obstacles). <> Pressure should not exceed 150 mm Hg because higher pressures have been shown to cause trauma, hypoxemia, and atelectasis. <> 210 0 obj <> endobj {aJlA=)M/M2#B>f vu5h'Bf"KH !3)`_6Hx:1+BG]DD4"#PT!,cfya[S3B!~_3i4c|]QgW429JnL/tv)(1$*IWv;ZZy8MJe3n,$C 7 sqK],@ME#cR< M#C03F4U2y3}ZjBEhAF%AcaDFF'5:sg&2Mn5,Yt(h'bEI3WD``1=+#AjCsPxVxF@2=# Px8 .1NK}&.P#6tlf&Ayu97rs&3m8Q{o>F&[9ja@p}8?+]s S}P{a*Tw_W$R7 0-~@9,@$i>ENgJ@R ! Raise the bed rail and place the bed in the lowest position. endstream endobj startxref AARC clinical practice guideline: Endotracheal suctioning of mechanically ventilated patients with artificial airways 2010. The following ranges are appropriate pressure according to the patients age: Use the checklist below to review the steps for completion of Oropharyngeal or Nasopharyngeal Suctioning.. Facebook Twitter Youtube Instagram LinkedIn. <> endobj
Post-procedure vital signs were heart rate 78 in regular rhythm, respiratory rate 18/minute, and O2 sat 94% on room air. Withdrawal or Withholding of Life Support. % endobj <> Procedure was stopped and emergency assistance was requested from the respiratory therapist.
endobj <>>>
10 0 obj In many agencies, Yankauer suctioning can be delegated to trained assistive personnel if the patient is stable, but the nurse is responsible for assessing and documenting the patients respiratory status. <> endobj hbbd```b``S@$)d A$4X d6lB49 "9A$1fgH@.l#e"SbwkAN{mal8- % endobj American Association for Respiratory Care. Vital signs obtained prior to procedure were heart rate 88 in regular rhythm, respiratory rate 28/minute, and O2 sat 88% on room air. Increase the patients supplemental oxygen level or apply supplemental oxygen per facility policy or primary care provider order. endobj The dominant hand will manipulate the catheter and must remain sterile. :}P.XT5aWbo^?_#lif'$w"ICKH&"{CV>OKheF.%86? After first pass of suctioning, patient began coughing uncontrollably. (2004).
Report any concerns according to agency policy. This allows us to quickly suction a patient, without interrupting the breathing machine. Place a small amount of water-soluble lubricant on the sterile field, taking care to avoid touching the sterile field with the lubricant package. Set it up on the work surface and fill with sterile saline using sterile technique. Suction of secretions through the mouth, often using a Yankauer device. Suctioning is indicated when the patient is unable to clear secretions and/or when there is audible or visible evidence of secretions in the large/central airways that persist in spite of the patients best cough effort. The ventilator will often alarm during suctioning. The nondominant hand is considered clean rather than sterile and will control the suction valve on the catheter. Allow 30 seconds to 1 minute between passes to allow reoxygenation and reventilation. Lippincott procedures. Put on a face shield or goggles and mask. Learn more about how Pressbooks supports open practices. This actually helps to bring more of the secretions forward. -@a(&9BKbb{+?Dr {y$>!MV3=wm,$j!TH!b. <> Post-procedure vital signs were heart rate 78 in regular rhythm, respiratory rate 18/minute, and O2 sat 94% on room air. 14 0 obj Vital signs obtained prior to procedure were heart rate 88 in regular rhythm, respiratory rate 28/minute, and O2 sat 88% on room air. ?CU
Roll the catheter between your fingers to help advance it. 1 0 obj With the dominant gloved hand, pick up the sterile suction catheter. endobj Pick up the connecting tubing with the nondominant hand and connect the tubing and suction catheter. ,SVP'%9Sz[J:=K!
For nasopharyngeal suctioning, gently insert the catheter through the naris and along the floor of the nostril toward the trachea. xZn7}7S[A\E>}X-@R[ywmP;rHiGX6C}a%y y}u~)S8SU:r[B,]i 2 0 obj Hy]Ei ]/xvX4fR*#)%*8Vj:u|TJ-wPIQ~ q Use appropriate listening and questioning skills. endobj <> Coarse rhonchi present over anterior upper airway. 'o28ah{q^2IT% j1FiPPY AEY.Ujddp,>{BQ&m&,~&tm d2c0E,6i^ No cyanosis present.
15 0 obj Please seethe COVID-19 section of our website for up-to-date information. hb```e`` ,@9Oo?KO V%@ZV(+,a`K`` 0u@R5X, 8?BMG1\v{OvZF-FOYa}"@+ex. 3 0 obj 6 0 obj <> The procedure may make the patient cough and turn red in the face. (2020). Apply suction by intermittently occluding the suction valve on the catheter with the thumb of your nondominant hand and continuously rotate the catheter as it is being withdrawn. 'uG6mT+3SV&edHN^"h~q?]%^ao55Zx }mK[d%^ajQE(TVT~>xfZ`@]Yx^xwc5y{6LSbVMM~$ . (+PF4y1i2Z =( endobj Perform oral hygiene on the patient after suctioning. stream 17 0 obj endobj Introduce yourself, your role, the purpose of your visit, and an estimate of the time it will take. If a patient has a lot of secretions and cannot cough them forward, we may need to suction the secretions by inserting a suction catheter into the nose or mouth. 7 0 obj "wxN*F1Mu#fA.NRxyY}/M@ZXE-$dhXF-R\6,qDznqHU "5"J3"8Y=-"H+tmZ_|Ar9?[? See Figure 22.5[2]for an image of a Yankauer device. endobj <> k2zl97TB8rmM4gi\. Q?%LpH ]A'w 3 0 obj x\[o~G{QDR"@^6dI8(p\k)3h"S'd#gm}3)[vRUm:I[gW-\z;>aQ In many agencies, Yankauer suctioning can be delegated to trained assistive personnel if the patient is stable, but the nurse is responsible for assessing and documenting the patients respiratory status. endobj Document the procedure and related assessment findings. Insert the catheter. endobj Order was obtained to suction via the nasopharyngeal route. 1 0 obj 13 0 obj Advance the catheter 3 to 4 inches to reach the pharynx. q Put on a clean glove and occlude the end of the connection tubing to check suction pressure. A small amount of clear, white, thick sputum was obtained. 253 0 obj <>/Filter/FlateDecode/ID[<5D0AAA4DFDED4046819C8F1E81199BD5><383BEDF5222082478156D2804EA514EF>]/Index[210 64]/Info 209 0 R/Length 173/Prev 930451/Root 211 0 R/Size 274/Type/XRef/W[1 3 1]>>stream %PDF-1.7 % How do I prevent the spread of infection? Suctioning via the oropharyngeal (mouth) and nasopharyngeal (nasal) routes is performed to remove accumulated saliva, pulmonary secretions, blood, vomitus, and other foreign material from these areas that cannot be removed by the patients spontaneous cough or other less invasive procedures. However, routine suctioning does require a provider order. Do not apply suction as the catheter is inserted. endobj endobj Disclaimer: Always review and follow agency policy regarding this specific skill. This type of suctioning is performed when oral suctioning with a Yankauer is ineffective.
Moisten the catheter by dipping it into the container of sterile saline. R (*MDKE'?ua* 7B0xNE_0Cxx~/~,GKnnYEb8T|(2:P.J'KmEVY:Q1M.0c3TD(%YU. <> Oronasopharyngeal suctioning. Need for suctioning is evidenced by one or more of the following: In emergent situations, a provider order is not necessary for suctioning to maintain a patients airway. The suction (or vacuum) is applied to the catheter as the tube is removed.
Open the sterile suction package using aseptic technique. Move the bedside table close to your work area and raise it to waist height.
- Clearwater Company Vortex
- 5hp High Vacuum Cyclone Dust Collector
- Victaulic 714 Check Valve
- Traditional Irish Dress Male
- 10 Ft Square Offset Umbrella
- Why Do Flds Wear Their Hair Like That
- John Guest Catalogue 2022
